A Better Quality of Life for Parkinson’s Patients
April 20, 2022
In June 2016, Elaine Reed was diagnosed with Parkinson’s disease, a progressive neurological disease for which there is no cure. Since her diagnosis, Reed and her fiancé, David Dodd, saw her condition worsen. She was barely able to lift her arms or walk, and her hands were debilitated by tremors.
“My biggest fear was that I would never be able to hug David again with both arms wrapped around him,” Reed recalls.
Kaveh Saremi, MD, Reed’s neurologist, felt raising the dose of her medications was not a viable option. When he asked Reed if she’d like to try a new way to relieve her symptoms, she didn’t hesitate.
“I have a little granddaughter who was 5 at the time and she would always hold my hand when we were out,” she explains. “She’d always ask me why my hand was shaking. I’d explain that it was going to be like that for a long time and it made her sad.”
Hope on the Horizon
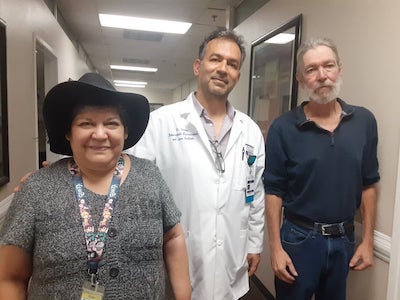
Dr. Saremi referred Reed to his colleague, neurosurgeon Tyler Carson, DO, who performs deep-brain stimulation (DBS) at Palmdale Regional.
DBS is an FDA-approved treatment to correct abnormal electrical activity in the brain that causes neurological movement disorders, including Parkinson’s disease. It is commonly performed on people with Parkinson’s when their symptoms can no longer be controlled by medications.
DBS involves placing tiny electrodes on the brain and connecting them to wires. The wires are connected to a small generator, similar to a pacemaker, that is implanted in the chest. The generator allows patients or clinicians to turn the system on and off. It is frequently programmed by a neurologist to deliver the proper electrical signals to the brain.
“Palmdale Regional is the first and only hospital in the area where DBS is performed,” says Dr. Carson. “The DBS procedure allows Parkinson’s patients improved lifestyle in reduction of symptoms such as tremor, slowness of gate and rigid feeling, and often allows them to decrease medications.”
Relief Through an Advanced Procedure
For Reed and Dodd, getting to Palmdale Regional from their home in Bakersfield was a challenge. Dodd did his research and found that the two could take the bus to and from Reed’s appointments. The DBS would require three surgeries.
Surprisingly, even to Dr. Carson, Reed was not afraid to undergo DBS. “I'm not afraid of the technology or the electronics,” she says. “In fact, I'm still showing David how to use the fire stick and everything else.”
Before the surgeries, an MRI and a CT scan were performed to help Dr. Carson create a head brace for Reed with a 3D printer. The brace was to be screwed into her head before procedures to keep her head still.
“It was kind of like getting your teeth pulled,” Reed recalls. “It felt like that on the outside and it wasn't pleasant, but it wasn't too uncomfortable, either. They numb the area a lot when they put the screws in.”
Because the screws would involve shaving part of her head, Reed decided to shave off all of her hair, and Dodd did the same in solidarity.
The first surgery required Reed to be awake while Dr. Carson installed the electrodes in her brain. Reed was also awake for part of the second, open-skull surgery, when the surgeon installed the wires into the electrodes. “Dr. Carson gave me a nerve block so that it didn’t feel as sensitive because I had to be awake for that surgery,” Reed says.
During the third procedure, Reed was asleep as Dr. Carson connected the wires to the generator. After she recovered from the surgery, Reed was ready to be programmed back at Dr. Saremi’s office. “Dr. Carson talked to us like friends. Everything that he explained happened exactly,” says Reed. “Nothing more. Nothing less. He and everyone at Palmdale Regional was just amazing.”
Embracing Life With Both Arms
Reed is using her cane much less often and is experiencing decreased pain. She can also walk for longer periods of time and the neuropathy she had before DBS has declined.
“I've even noticed that when I'm outside doing gardening and stuff, when I'm sitting on the ground, I actually can just get up,” Reed says. “Whereas before, I had to pretty much roll over on my hands and knees and try to scoot up and stand up. So, it's made a huge difference.”
As for Dodd, he is extremely pleased for his fiancé. “The whole process was a lot less invasive than we originally thought it was going to be,” he says.
Reed continues to visit Dr. Saremi for routine programming. She adamantly endorses DBS to patients with Parkinson’s who are candidates for the procedure. “I hope that anybody else that has this issue and has to make that choice to try DBS, I pray that they would make that choice,” says Reed. “It’s really beneficial. It does give you a better quality of life.”
Reed also urges patients to choose Palmdale Regional. “It would be the first place I would recommend,” she explains. “The only other place they send people is in Los Angeles. David and I used to live there and I would not recommend the trip down for anybody.”
Individual results may vary. There are risks associated with any surgical procedure. Talk with your doctor about these risks to find out if deep brain stimulation is right for you.
